Personally, I would have liked to have just added the link to this article, as it is fairly lengthy. It is, however, very important for each person to read. We never know when this information can or will be pertinent.
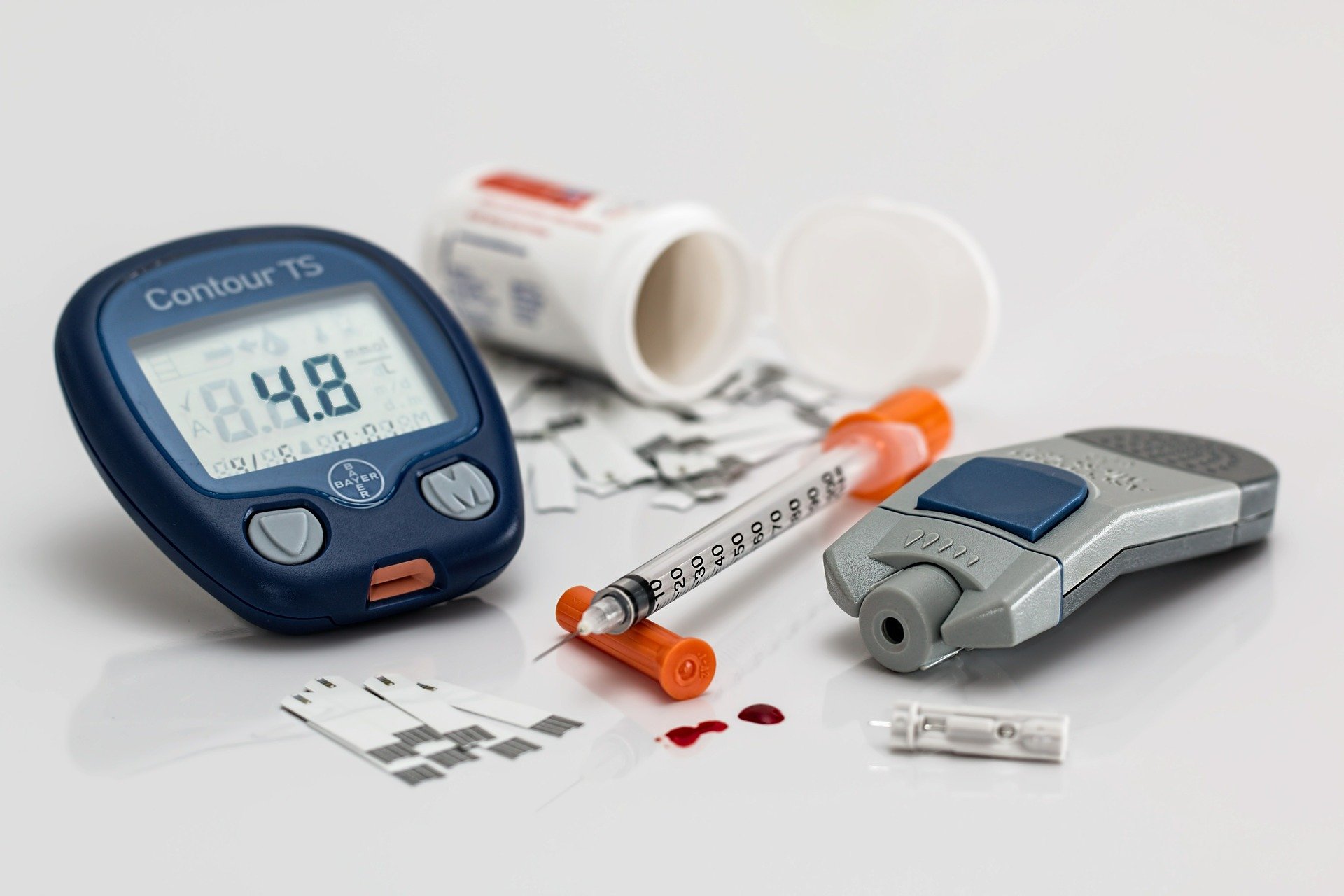
I personally encountered a woman in a Diabetic crisis in a gas station last year. Knowing what to do, prevented her from going into s severe reaction and needing an ambulance. Sadly, everyone else just stood around. I was thankful I recognized the signs and was able to help her immediately. My Mother-In-Law is and Best Friend, are both Diabetic, so this information becomes especially important within our family. When this situation occurs, we have minutes to respond, not hours. It must be attended to immediately.
Posted by Prepper Ideas | Posted on 03-31-2014
Patient Information
Modern media have made our world seem small. News about events around the world reaches us in minutes. We learn of hurricanes, floods, earthquakes, volcanic eruptions, industrial accidents and terrorist attacks immediately. TV teaches us that any disaster brings chaos to people and their environments.
As a person with diabetes, your daily routine involves schedules and planning. An emergency can seriously affect your health. It may be difficult to cope with a disaster when it occurs. You and your family should plan and prepare beforehand even if the event is loss of electricity for a few hours. The first 72 hours following a disaster are the most critical for families. This is the time when you are most likely to be alone. For this reason, it is essential for you and your family to have a disaster plan and kit which should provide for all your family’s basic needs during these first hours.
Be Prepared List
You should safely store the following medical supplies or have them readily available:
- Copy of your emergency information and medical list
- Extra copies of prescriptions
- Insulin or pills (include all medications that you take daily including over the counter medications)
- Syringes
- Alcohol swabs
- Cotton balls & tissues
- A meter to measure blood sugar
- Blood sugar diary
- Insulin pump supplies (if on insulin pump)
- Strips for your meter
- Urine ketone testing strips
- Lancing device and lancets
- Quick acting carbohydrate (for example, glucose tablets, orange juice, etc.)
- Longer lasting carbohydrate sources (for example, cheese and crackers)
- Glucagon Emergency Kit (if on insulin)
- Empty hard plastic detergent bottle with cap to dispose used lancets and syringes
Other supplies:
- Flashlight with extra batteries
- Pad/pencil
- Whistle/noisemaker
- Matches / candles
- Extra pair of glasses
- First-aid kit
- Female sanitary supplies
- Copy of health insurance cards
- Heavy work gloves
- Important family documents
- Tools
- Water
- Food
- Clothing and bedding
- Radio with extra batteries
- Cell phone
Make sure you have enough supplies for 2 weeks. These supplies should be checked at least every 2 – 3 months. Watch for expiration dates.
Helpful hints about insulin, pens, syringes
- Insulin may be stored at room temperature (59° – 86°F) for 28 days.
- Insulin pens in use can be stored at room temperature according to manufacturer’s directions.
- Insulin should not be exposed to excessive light, heat or cold.
- Regular and Lantus insulins should be clear.
- NPH, Lente, Ultralente, 75/25, 50/50, and 70/30 insulins should be uniformly cloudy before rotating.
- Insulin that clumps or sticks to the sides of the bottle should not be used.
- Although reuse of your insulin syringes is not generally recommended, in life and death situations, you have to alter this policy. Do not share your insulin syringes with other people.
Things to remember
- Stress can cause a rise in your blood sugar.
- Erratic mealtimes can cause changes in your blood sugar.
- Excessive work to repair damage caused by the disaster (without stopping for snacks) can lower your blood sugar.
- Excessive exercise when your blood sugar is over 250mg can cause your blood sugar to go higher.
- Wear protective clothing and sturdy shoes.
- Check your feet daily for an irritation, infection, open sores or blisters. Disaster debris can increase your risk for injury. Heat, cold, excessive dampness and inability to change footwear can lead to infection, especially if your blood sugar is high. Never go without shoes.
Hot weather tips
- Stay indoors in air-conditioned or fan cooled comfort.
- Avoid exercising outside.
- Wear light colored cotton clothing.
- Remain well hydrated (water, diet drinks).
- Avoid salt tablets unless prescribed by your physician.
- Seek emergency treatment if you feel: Fatigue, weakness, abdominal cramps Decreased urination, fever, confusion.
You should wear diabetes identification at all times.
Food items to be stored
- 1 large box unopened crackers (saltines)
- 1 jar peanut butter
- 1 small box powdered milk (use within 6 months)
- 1 gallon or more of water per day per person for at least one week
- 2 6-pack packages cheese and crackers or 1 jar soft cheese
- 1 pkg. dry, unsweetened cereal
- 6 cans regular soda
- 6 cans diet soda
- 6-pack canned orange or apple juice
- 6 pack parmalat milk
- 6 cans “lite” or water packed fruit
- 1 spoon, fork and knife per person
- Disposable cups
- 4 packages of glucose tablets or small hard candies for low blood sugar
- 1 can tuna, salmon, chicken, nuts per person
These supplies should be checked and replaced yearly.
Food considerations during a disaster
- Food and water supply may be limited and/or contaminated. Do not eat food you think may be contaminated. It may be necessary to boil water for 10 minutes before use.
- Drink plenty of water.
- Maintain your meal plan to the best of your ability. Your plan should include a variety of meat/meat substitutes (i.e., peanut butter, dried beans, eggs), milk/milk products, fruits, vegetables, cereal, grains.
- Limit sugar/sugar-containing foods. These foods include:
- Jellies, jams, molasses
- Honey
- Syrups (fruits canned in sugar syrup, pancake syrup)
- Tonic (dietetic tonics with less than one calorie per ounce are allowed)
- Frosted cake
- Presweetened or sugar-coated cereals
- Pie, pastry, Danish pastry, doughnuts
- Chocolate
- Custards, pudding, sherbet, ice cream
- Gelatin
- Soda
- Cookies, brownies
5. Monitor your blood sugars frequently and record in diary.
Limit sweets.
6. When reading labels, limit products with these sugar-containing ingredients:
- Sugar
- Corn syrup
- Dextrose
- Sucrose
- Corn sweeteners
- Honey
- Molasses
- Brown sugar
- Fruit syrup
7. Avoid greasy, fried foods.
8. Try to eat meals and snacks at the same time every day. Avoid periods of hunger and overindulgence. The quantity and frequency of your food intake should remain similar day-to-day depending upon your activity level.
9. Increase food and water intake during periods of increased exertion or physical activity by either eating between-meal snacks before activity or by eating additional food with meals.
10. Carry a fast source of sugar with you at all times:
- 3 glucose tablets
- 1 small box of raisins
- 6-7 small hard sugar candies
Sick day rules during a disaster
- Always take your insulin or pills on time or close to it. Never omit your insulin unless your doctor has told you otherwise. Insulin is still good if there is no refrigeration. A used or unused bottle of insulin may be kept at room temperature (59° – 86°F) for 28 days. Discard unrefrigerated insulin after 28 days.
- Keep an extra bottle of each type of insulin you use on hand at all times.
- Eat within 15 min. or no later than ½ hour after taking your insulin
- (depending on insulin type) or diabetes medicine. Try to eat on time.
- Never skip a meal. If you cannot eat solid food because of nausea, vomiting, and/or diarrhea, sip regular coke, eat hard candies, fruit or regular soft drinks instead of following your usual meal plan.
Most Important:
- Do not let yourself get dehydrated.
- Drink plenty of liquids.
- In between meal times, sip diet soda.
(This will not replace food, but can help you be hydrated.)
6. Rest.
7. Check your blood sugar. Notify your doctor if your blood sugar average is over 240mg or if you are ill for 2 days.
8. Test your urine for ketones when:
- Your blood sugar average is over 240mg.
- You are vomiting
- You have symptoms of high blood sugar (increased thirst or hunger than usual, quick weight loss, increased urination, very tired, stomach pain, breathing fast or fruity breath smell).
9. Call your doctor if your ketone test is moderate or high and/or if you have symptoms of high blood sugar (as listed in number 8). You may need more than your usual amount of insulin on a sick day. Your doctor can guide you in this. If you need medical assistance / or are out of all medications, food, and cannot reach your doctor, immediately:
- Go to the nearest hospital; or
- Contact the police; or
- Contact the American Red Cross; or
- Go to an Emergency Medical Center